Abstract
Introduction: Real-world survival for pts with MDS treated with HMAs is substantially inferior than the landmark AZA-001 trial (median OS, 11-16 and 24.5 months, respectively). The reasons behind this gap remain unclear. Clinical use of HMAs differs from traditional chemotherapy in that multiple HMA cycles are generally required before responses are observed, therapy is continued even in the presence of significant cytopenias, and therapy must be continued to sustain response. We hypothesized that practice at academic hospital setting or prior experience of providers in treating MDS pts (more specifically the number of pts initiated on HMAs) are positively associated with persistence in HMA therapy and improved OS.
Methods: Using SEER-Medicare linked data, we identified MDS pts diagnosed in 2004-13. Inclusion criteria included being ≥66 years at diagnosis, continuous Medicare Parts A&B coverage, and ≥ 1 full HMA cycle (defined by 3-10 days of HMA use within 28 days). Pts were followed until death or December 31, 2014. We identified the physician associated with HMA initiation, and assessed that provider's prior experience in caring for MDS pts or in initiating HMAs in a 2-year lookback period. Only pts diagnosed with MDS and initiated HMA in 2006-2013 were included for analysis to allow 2-year lookback for volume calculation. MDS volume and HMA volume were categorized into dichotomous variables given their skewed distribution (0-14 vs. 15 or more for MDS volume, 0 vs. 1 or more for HMA volume). Provider type was defined based on claim type (hospital outpatient [HOPD] or community provider) and linked information on hospital characteristics as 1) HOPD, teaching or cancer center (academic) or 2) HOPD, neither teaching hospital nor cancer center (HOPD-nonacademic) and 3) community-based practice. We assessed HMA duration as number of cycles of HMA therapy, with cycles separated by a gap of >= 2 weeks without therapy. We calculated OS from the first day of HMA. Chi-squared tests were used to assess differences in proportion of pts receiving ≥4 HMA cycles, and proportion with 2-year survival across different levels of HMA volume, MDS volume, and provider types. Wilcoxon rank sum test and Kaplan-Meier (KM) log-rank test was used to examine distribution of HMA cycles and OS across different levels of volume and provider types. Finally, we used multivariate Cox proportional hazards model to analyze OS, and similarly multivariate logistic regression for duration of HMA treatment, both of which were adjusted for relevant covariates (see footnote of Figure 1 for covariates). Two-sided statistical tests were used with alpha=0.05.
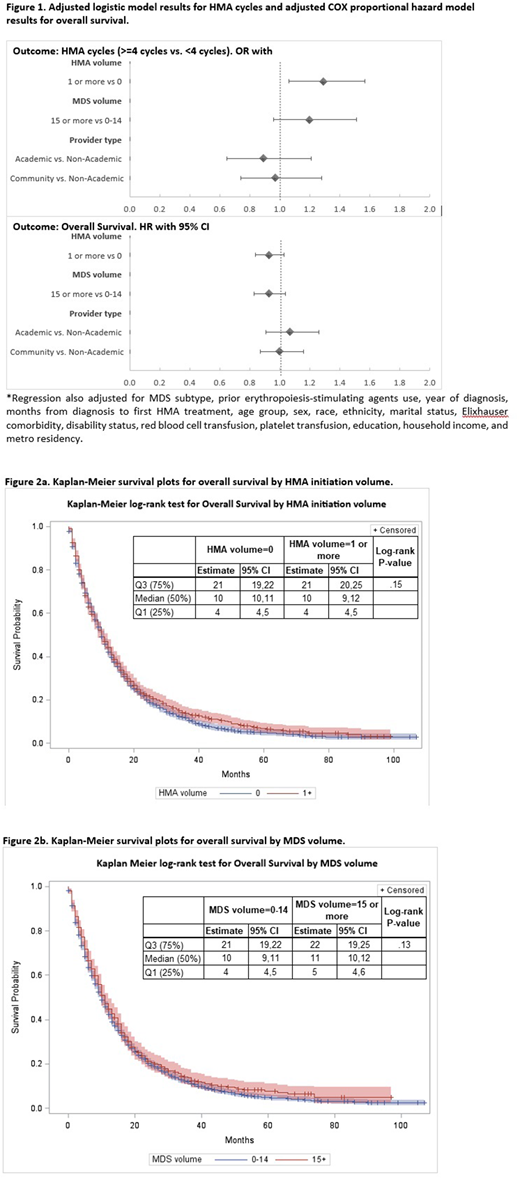
Results: We identified 2,128 eligible pts under the care of 1,157 providers with 2-year lookback period. Median age at diagnosis was 77 (interquartile range 72-82) years, and 90.2% of patients were white. Median number of HMA cycles was 4, and median OS was 10 months (95% CI: 10-11). Median MDS volume was 8 and 32.2% of pts' providers had at least 1 HMA initiation in the past 2 years. Pts treated by provider with MDS volume ≥15 or with HMA initiation volume ≥1 are more likely to receive ≥4 HMA cycles in unadjusted analyses (P=.03 and P=.002 respectively). Community providers had significantly higher percentage of ≥ 1 HMA initiation than either group of HOPD hospital providers (P<.001). However, no differences were found between HOPD academic vs. HOPD non-academic (P=.17). In adjusted logistic regression analysis, we found that pts whose provider had ≥ 1 HMA initiation in the past year are more likely to receive persistent HMA (OR=1.29, 95% CI=1.06-1.57, P=.01, [Figure 1]). No significant association was found between MDS volume and persistent HMA therapy. KM analyses indicated no significant differences in OS across different levels of MDS volume or HMA initiation volume [Figure 2].
Conclusions: MDS pts whose providers were more experienced with HMA had higher odds of receiving persistent HMA than pts with less experienced providers. However, there was no difference in the OS based on provider experience. These findings suggest specialized care of MDS pts can decrease inappropriate early discontinuation of HMA therapy, but does not seem to improve OS. Further research into the underlying reasons for the gap in OS between HMA-treated pts observed in clinical trials compared to real-life setting is warranted to help develop interventions to improve outcomes at the population setting.
Zeidan:Celgene: Consultancy; Pfizer: Consultancy; Novartis: Consultancy; Incyte: Employment; Gilead: Consultancy; Abbvie: Consultancy; Agios: Consultancy; Ariad: Consultancy, Speakers Bureau. Huntington:Bayer: Consultancy; Celgene: Consultancy; Janssen: Consultancy. Podoltsev:Celator: Research Funding; Astellas Pharma: Research Funding; Boehringer Ingelheim: Research Funding; Daiichi Snakyo: Research Funding; Pfizer: Membership on an entity's Board of Directors or advisory committees; Genentech: Research Funding; Astex Pharmaceuticals: Research Funding; Celgene: Research Funding; Sunesis Pharmaceuticals: Research Funding; Pfizer: Research Funding; LAM Therapeutics: Research Funding. Gore:Celgene: Consultancy, Research Funding. Ma:Incyte: Consultancy; Celgene: Consultancy. Davidoff:Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal